HIMSS Proposes a New Interoperability Definition in Healthcare
As the healthcare industry evolves, so do concepts like interoperability. In its latest evolution, HIMSS is proposing a new interoperability definition in healthcare. So what does this mean for the healthcare industry?
Interoperability, which has become a heavily-discussed topic in healthcare, describes the ability for information systems to connect across organizational boundaries – simply put, systems are interoperable when they can transfer information smoothly among one another. There are numerous benefits to having an interoperable organization, including:
- Greater efficiency
- Reduced waste, costs, and errors
- Reduced patient frustration
- Streamlined care coordination
- Support for value-based care initiatives
- Enhanced quality analytics and more effective research
- Improved patient care
What’s New About the Definition of Interoperability?
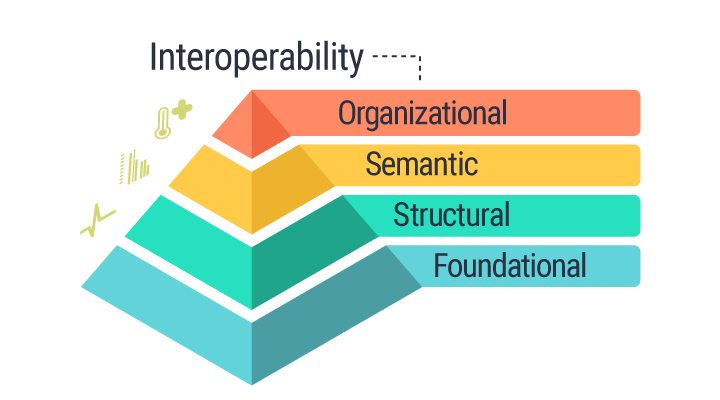
Currently, HIMSS classifies interoperability as having three components: foundational, structural, and semantic. Now, the group is proposing a fourth type: organizational interoperability. The goal, according to Mari Greenberger, Senior Director of Informatics at HIMSS, is to consider a global perspective of interoperability so that information can be shared seamlessly across borders and jurisdictions.
“This definition is an aspirational one. It’s what HIMSS is trying to accomplish and work toward when it comes to achieving global interoperability. We added the additional level of ‘organizational’ to illustrate the critical need for a robust interoperability infrastructure as well as highlighting the non-technical considerations that play into successful interoperability.” – Mari Greenberger
Components of Interoperability
To better understand how interoperability works, think of the individual stages as a pyramid with “foundational” at the bottom and “organizational” at its zenith.
- Foundational interoperability represents the building block of information exchange. It establishes interconnectivity requirements so that systems can connect and exchange data between one another, but it doesn’t require the receiving technology to be able to interpret the data.
- Structural interoperability is the structure or format of the information exchange. Serving as a middle layer, it’s the syntax of data exchange, focusing on how data is packaged via message format standards. It ensures that the clinical purpose and meaning of the data being exchanged is unaltered and preserved.
- Semantic interoperability is one of the highest levels of data exchange. This assures that multiple systems can transfer and use information through uniform terminology.
Because healthcare organizations use varying EHR systems, their information is represented differently, which can cause interoperability issues. But with semantic interoperability, disparate systems can share data in a streamlined way by creating a common vocabulary that ushers in reliable communication between systems.
“While a doctor knows that ‘dropsy’ describes the same illness as congestive heart failure, a computer typically can’t make that distinction. Semantic interoperability, however, aims to create a common vocabulary that will pave the way for accurate and reliable communication among computers.” – Timothy Cook, Health Language Blog
Organizational interoperability is the newest proposed tier. Encompassing technical, policy, and social elements, HIMSS stated this new addition to the definition of interoperability “facilitate[s] the secure, seamless and timely communication and use of data within and between organizations and individuals.”
HIMSS commented that this change was proposed to support relationships, efficiency, and overall wellness across organizational boundaries.
“In the health ecosystem, interoperability furthers the goal of optimizing health by providing seamless access to the right information needed to more comprehensively understand and address the health of individuals and populations,” HIMSS continued.
This topmost tier represents the most challenging parts of implementing interoperability: the non-technical consideration of policy, cultural, regulatory, workflow, and other changes necessary for seamless data flow.
What does this mean for the healthcare industry?
Systems can exchange healthcare data with varying degrees of interoperability. One or more of the components above can be used when exchanging PHI between organizations. Although complex, the proposed changes to interoperability were made with expansion in mind – when information can cross borders, patients can enjoy even more streamlined care.
With the proposed addition of an organizational layer, interoperability in healthcare would become even more comprehensive. At its most optimal level, information exchange can be integrated across both systems and borders regardless of origin. The goal is for data to be both usable and readily available without user intervention. With the ability of information to cross borders becoming more clearly defined, interconnectivity of health data can expand to a global scale, able to better address the health of individuals all the way to entire populations.
