How to Successfully Improve your Clinical Communications: Empower your Crew
If you are looking to improve clinical communications across your hospital, you are certainly not alone. The productivity and economic impact of inefficient communication (and the subsequent effect on patient care) has been well-documented, leading many hospitals, ambulatory clinics, and long-term care coordinators to move away from pagers in favor of more modern, efficient solutions.
It can be difficult, however, to find useful advice for how to make these improvements when hospital environments are so unique. No two hospitals are the same, and therefore, no two projects are the same.
For many hospitals, the biggest challenge is getting the right people in the room. If you are deploying new clinical communication tools, you need to build your “dream team”. One of the most common pitfalls we see is passing a project off to the IT team without any involvement or support from clinical stakeholders.
Think of your current inefficient communications as a large body of water to cross. Building the right implementation team is the best way to get from point A to point B. At the most basic level, you have your IT team. It will provide the physical structure for a ship, and they will do the technical work of implementing your solution. But you can’t leave the project at that – because the IT team many not know where point B is.
You need clinical influence to provide an understanding of the current workflows and the role of communications. This understanding gives your ship direction. While your IT resources might have a full grasp of the technology to provision and support your users, they may not have the same insight on use cases that clinicians can identify. Providers themselves are needed to point out the various inefficiencies in their current communications paths. As you start implementing a more efficient secure communications solution, it is especially important to identify these pain points and develop new workflows around them.
During this time, you can leverage your clinical advocates to understand both the roles and the tools involved in these workflows. For example, when prescribing medication, physicians might be responsible for entering an order, but when there are any verification questions, pharmacists and charge nurses will also likely be brought in.
Clinical advocates will also understand the different tools and technologies used for communications in their current workflows. Often, existing workflows use a variety of different communication methods that can vary depending on specific providers’ preferences. Providers move between different outdated technologies for a single workflow, which wastes time. The infographic below depicts the order verification workflow using current inefficient technologies: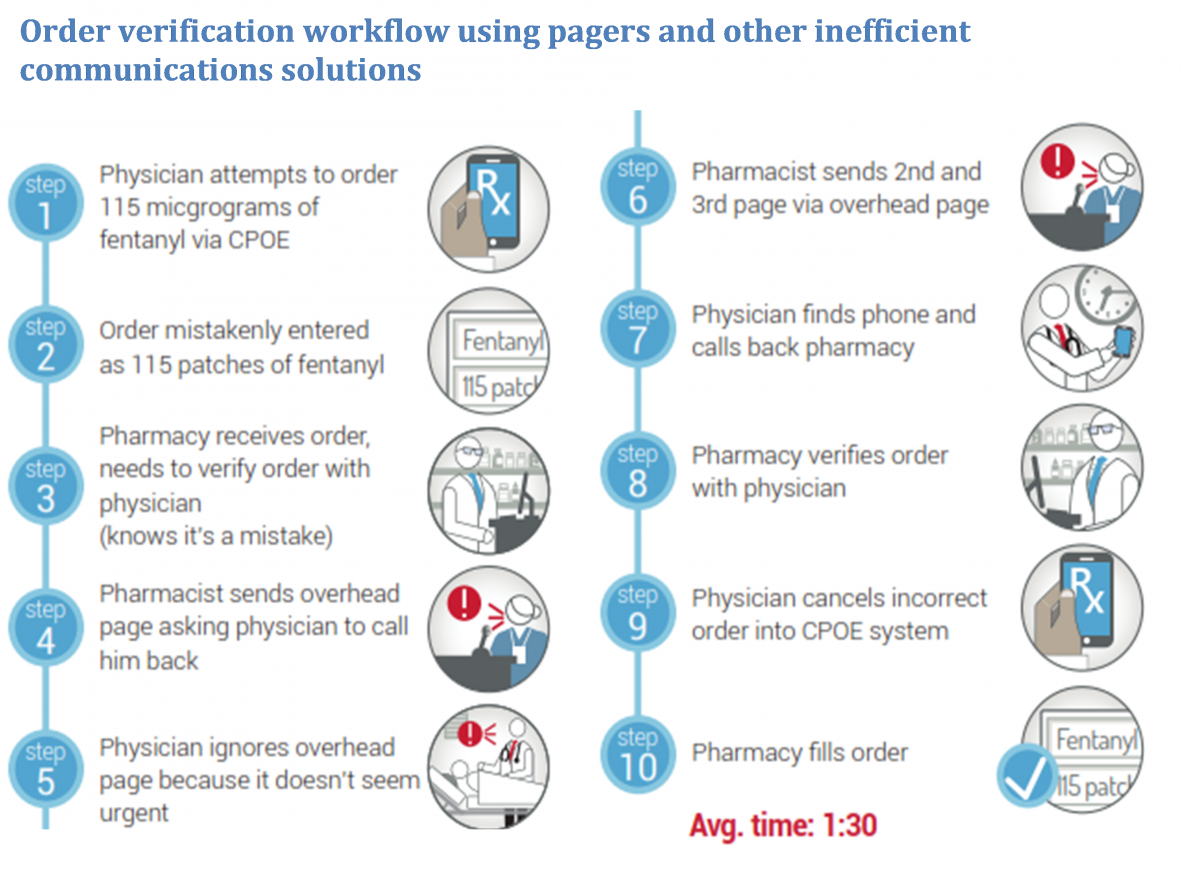
By working with your clinical team to identify all the different moving parts in these processes, you can better understand how to improve communications and streamline workflow.
In addition to the clinical involvement, you’ll also need engagement from leadership. This is the fuel for your ship. Without this support, you won’t be able to move forward. If there’s one thing that all hospitals have in common, it’s that they are always juggling competing projects. If you neglect to show any executive support in your new communications implementation, then you will be unlikely to see the success and adoption you need to make an impact.
Improving clinical communications is a challenge, but with the right perspective and planning, you can greatly improve day-to-day clinical workflows. As you begin this endeavor, consider the team you’ll need to empower to introduce your solution effectively. Hospitals across the world are taking the time and resources to replace their outdated technologies, and introduce new, time-saving workflows.
If you don’t, you may be left at the dock.
